Health Advice
/Health

The retiree’s year-end wellness checklist for a healthier 2026
Don’t wait until Jan. 1 to scramble for health resolutions that rarely last. As you enter a new year, the focus should shift from just “being healthy” to optimizing your longevity and vitality. Maintaining physical health, preventing cognitive decline, and building social resilience are paramount to a happy and active retirement.
Use this...Read more

Environmental Nutrition: Freezer rules
Q: How long can I safely freeze certain foods?
A: Freezing food is a smart way to cut waste and save time, but even frozen food has limits on quality. While frozen items kept at 0 F (-18 C) remain safe indefinitely, their taste and texture can suffer over time.
Meats like beef steaks or whole chicken maintain best quality for up to 12 months. ...Read more

Does eating fruit help with weight loss?
Eating fruit can help you lose weight, particularly if you choose fruit rather than processed foods that are high in added sugar and fat. Making fruit a daily staple in your diet can offer many health and nutritional benefits. The high fiber content can help you feel full, and the natural sweetness can help stave off cravings.
Fruit often gets ...Read more

Mind your heart for a longer, healthier life
Stories about people with remarkably long life spans — like the Spanish woman who died at the age of 117 earlier this year — often spark speculation about longevity secrets. They’ve also fueled the growing interest in longevity clinics. But what does the science actually say?
“There are plenty of affordable, proven strategies to live a ...Read more

Mayo Clinic Q&A: Emotional exhaustion: When your feelings feel overwhelming
DEAR MAYO CLINIC: Recently, I’ve been feeling physically and mentally drained from the demands of work, caregiving and other responsibilities. I struggle to find motivation and have trouble concentrating on tasks. Are there strategies to help me find emotional balance?
ANSWER: Turning on the news or opening a newspaper to see local and world ...Read more

Get to know your microbiome: It can improve gut health and more
ROCHESTER, Minn. — Resolutions to improve health typically include measures such as more exercise, a healthier diet and stopping smoking. But what about your gut microbiome? Taking steps to protect and improve it can benefit digestive health and more, says Purna Kashyap, M.B.B.S., a gastroenterologist at Mayo Clinic who specializes in the gut ...Read more

Bill of the month: Scorpion peppers caused him 'crippling' pain. Two years later, the ER bill stung him again
Maxwell Kruzic said he was in such “crippling” stomach pain on Oct. 5, 2023, that he had to pull off the road twice as he drove himself to the emergency room at Mercy Regional Medical Center in Durango, Colorado. “It was the worst pain of my life,” he said.
Kruzic was seen immediately because hospital staff members were pretty sure he ...Read more

Rural health is a 'real concern,' Gov. Little says. Idaho to get millions to help
Idaho is set to receive over $900 million in federal money over the next five years to improve the state’s provision of healthcare in rural areas, Gov. Brad Little’s office announced. The funds were allocated as part of the Rural Health Transformation Program under House Resolution 1, also called the One Big Beautiful Bill Act.
“For many ...Read more

Salmonella outbreak update: Maryland cases, hospitalizations increase
BALTIMORE — Since the Centers for Disease Control and Prevention released its initial report on a recent outbreak of a strain of Salmonella linked to raw oysters, cases and hospitalizations in Maryland have seen a slight increase.
On Dec. 23, the CDC reported one Maryland resident as having fallen ill after being infected with the strain. In ...Read more

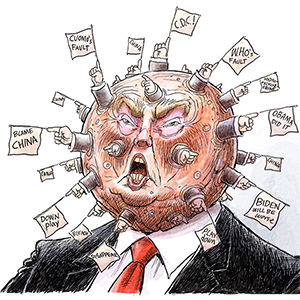
Health care fight returns in January with affordability at center
WASHINGTON — Health care policy will be top of mind when Congress returns to Washington in January, with lawmakers acknowledging that escalating insurance premiums are hitting millions of Americans.
That’s about where the agreement ends. The parties and even the factions within them are sharply divided on the path forward — with several ...Read more

Texas gets largest share of reconciliation law's rural health fund
The Trump administration on Monday announced that all 50 states will receive proceeds from a $50 billion rural health fund, the creation of which helped secure the support for President Trump’s tax cuts law from Republican senators worried about the impact of Medicaid cuts in their states.
In 2026, the first year of the program, states will ...Read more

Coloradans snap up over-the-counter naloxone while hospitals offer the overdose-reversal drug to more patients
DENVER — Colorado is coming closer to universal access to overdose-reversing medication as residents snap up an over-the-counter version and hospitals offer it to more patients.
Naloxone, sold under the brand name Narcan, counters the effect of opioids so that a person who is overdosing doesn’t stop breathing. For the last decade, Colorado ...Read more

A couple told patients they'd created a breakthrough medical device. In a Philadelphia courtroom, they admitted it was all a lie.
She went by Dr. Mary, and her promise was a tantalizing medical breakthrough.
At clinics operated in Arizona and several other states, Mary Blakley and her husband, Fred, told patients that for just $300, they could provide a full-body scan that utilized a proprietary "smart chip" to detect a variety of potential illnesses, including cancer.
...Read more

Kentucky to receive $212.9M from feds to strengthen rural healthcare
Kentucky will receive $212.9 million from President Donald Trump’s administration over the next five years to improve rural health care, state officials said Monday.
The money will be used to address stubborn, long-term rural health care problems including maternity care deserts, limited access to mental health professionals and gaps in oral ...Read more

Trump rural health grants come with clawback threat to states
The Trump administration is announcing awards to states from a rural healthcare fund, with the threat that some of that money can be clawed back if jurisdictions fail to embrace policy initiatives backed by the president.
The discretionary grants for 2026 range from $145 million to $281 million for states, according to Mehmet Oz, the head of ...Read more

Feds to award Illinois $193M next year for rural health care as part of big beautiful bill
The federal government is awarding Illinois $193 million next year to support rural healthcare — money that’s part of the One Big Beautiful Bill Act, but not enough to make up for Medicaid cuts from the measure, state health leaders say.
Illinois asked the federal government for $200 million a year for each of the next five years in its ...Read more

Maryland receives $168M to boost rural healthcare
WASHINGTON — Maryland will receive $168 million to bolster its rural healthcare services, the Centers for Medicare and Medicaid Services announced on Monday.
The money will be allocated from CMS’ Rural Health Transformation Program. The program is a five-year, $50 billion health care fund that was included in the One Big, Beautiful Bill to ...Read more

Health insurance costs spike for businesses, workers after pandemic
The cost of employer-sponsored health insurance in California rose at twice the pace of inflation over the past three years, squeezing workers’ paychecks and small businesses alike.
More than 17 million Californians have health insurance through their job, according to a survey released in November by the health information group KFF. The ...Read more

Ask the Pediatrician: Why bullying hurts all children and what parents can do about it
Every day, thousands of kids suffer the fear, shame and frustration of being bullied. More than 19% of children aged 12 to 18 say they have been targeted by peers, with a frightening number of cases happening online. Here's what every parent needs to know about bullying and the actions that can help stop it.
Kids can be cruel, as the old saying...Read more
Skyrocketing Affordable Care Act premiums are pushing some to extreme measures
Mary Jo Armstrong and her ex-husband, William, didn't exactly remarry for love. They remarried for health insurance.
After 18 years of marriage and a divorce, finalized in 2014, the Upper Burrell, Pennsylvania, couple found themselves side-by-side again Dec. 18. Joining them — not in a church or courthouse, but over a Microsoft Teams call —...Read more
Popular Stories
- Bill of the month: Scorpion peppers caused him 'crippling' pain. Two years later, the ER bill stung him again
- Get to know your microbiome: It can improve gut health and more
- Health care fight returns in January with affordability at center
- Mayo Clinic Q&A: Emotional exhaustion: When your feelings feel overwhelming
- Does eating fruit help with weight loss?