Current News
/ArcaMax

Trial underway for Northern California mom charged with running alcohol-fueled teen sex parties
SAN JOSE — After four years, dozens of criminal charges and a superseding indictment, a trial is fully underway for a Los Gatos woman notorious for allegations she hosted boozy and raucous teen parties for her son and his friends, and goaded them into performing inebriated and nonconsensual sex acts with girls who attended.
Shannon O’Connor...Read more

NYC Mayor-elect Mamdani names Sherif Soliman as budget director
NEW YORK — Mayor-elect Zohran Mamdani on Thursday named Sherif Soliman as his budget director, one of the most consequential roles at City Hall, as his administration seeks to follow through on its ambitious affordability agenda.
Soliman, a local government vet who previously served in the administration of former Mayor Bill de Blasio, will ...Read more
6 dead after plane owned by former NASCAR driver crash lands in North Carolina
Six people were killed when a small plane owned by former NASCAR driver Greg Biffle crash landed and exploded into flames at a regional airport in North Carolina on Thursday morning, authorities said.
Biffle, his wife, Cristina, and his two children, Emma and Ryder, were among those killed, according to family friend Garrett Mitchell. In a ...Read more

She was approved for a green card after 3 decades in the US. Then ICE arrested her
LOS ANGELES — Babblejit “Bubbly” Kaur and her husband, Amarjit Singh, celebrated their 41st wedding anniversary in Long Beach in late November. The pair cradled a mint-frosted cake in their hands and beamed as their daughter, Joti, snapped pictures.
The couple endured a lot in those years, more than 30 of which have been spent in the U.S....Read more
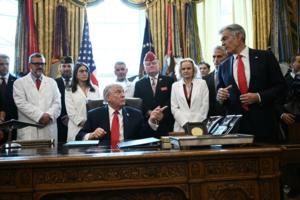
Trump eases restrictions on marijuana by executive order
President Donald Trump signed an executive order Thursday fast-tracking a push to ease some restrictions on marijuana in one of the most significant shifts in federal drug policy in decades.
The move aims to reclassify marijuana as a less-dangerous drug within a few months and opens new avenues for medical research, inching closer to the moves ...Read more
Plane owned by NASCAR driver Greg Biffle crashes while landing at Statesville airport in North Carolina
CHARLOTTE, N.C. — A plane crashed early Thursday at Statesville Regional Airport, about a 45-mile drive north from Charlotte, according to airport officials.
Iredell County Sheriff Darren Campbell said shortly before 1:30 p.m. that there were multiple fatalities, but he could not yet confirm the number. He said the sheriff’s office, North ...Read more

Miami Judge lifts block on Trump library land transfer, tosses Sunshine Law case
MIAMI — A judge on Thursday cleared the way for Miami Dade College to give up prime downtown land to be used for Donald Trump’s presidential library, tossing a case that alleged the college broke state law when trustees first voted to give away the Biscayne Boulevard parking lot to the state.
The decision clears the way for Trump’s ...Read more

Powerball jackpot jumps to about $1.5 billion, the seventh largest in history
The Powerball jackpot has soared to an estimated $1.5 billion for Saturday night's drawing, the fifth largest in game history and the seventh highest among all lottery jackpots in the United States.
The jackpot has an estimated cash value of $686.5 million, according to a Powerball news release.
No ticket matched all six numbers drawn ...Read more

Board votes unanimously to rename building Trump-Kennedy Center
White House press secretary Karoline Leavitt said Thursday that the board of the John F. Kennedy Center for the Performing Arts voted to change the name of the world-famous complex to the Trump-Kennedy Center.
“I have just been informed that the highly respected Board of the Kennedy Center, some of the most successful people from all parts of...Read more

Brentwood is mourning the Reiners, but also having OJ Simpson flashbacks
LOS ANGELES — Sandwiched between Bel-Air and Santa Monica, the tony Los Angeles neigborhood of Brentwood has long been home to more than its fair share of industry captains, actors, directors, musicians, media moguls and professional athletes.
But despite its tall hedges, multimillion-dollar homes and marquee names, residents say Brentwood ...Read more

Worried about health insurance costs? There may be cheaper options -- but with trade-offs
For the millions of Americans who buy Affordable Care Act insurance, there’s still time left to enroll for 2026. But premium increases and the expiration of enhanced tax subsidies have led to larger-than-expected costs.
Concerned shoppers, wondering if there’s anything they can do, are consulting insurance brokers or talking to ...Read more

Board votes unanimously to rename venue Trump-Kennedy Center
White House press secretary Karoline Leavitt said Thursday that the board of the John F. Kennedy Center for the Performing Arts voted to change the name of the world-famous complex to the Trump-Kennedy Center.
“I have just been informed that the highly respected Board of the Kennedy Center, some of the most successful people from all parts of...Read more

Racial profiling concerns grow as ICE expands presence in Twin Cities
MINNEAPOLIS — An 18-year-old Guyanese U.S. citizen had just finished a quick stop at a gas station near Hamline University in St. Paul when federal immigration agents approached him and demanded identification. His ID had expired, and the encounter quickly escalated into a tense standoff over proof of citizenship.
According to the student’s...Read more

Marathon hearings conclude in state case against Luigi Mangione in UnitedHealthcare CEO killing
NEW YORK — Marathon proceedings in Luigi Mangione’s state homicide case came to a close Thursday, as Manhattan prosecutors and lawyers for the suspected killer of UnitedHealthcare CEO Brian Thompson rested without calling any more witnesses.
The parties won’t learn for some time which positions prevailed, with state Supreme Court Justice ...Read more
Small plane owned by ex-NASCAR driver crash lands at NC airport
A small plane owned by a former NASCAR driver crash landed and exploded into flames at a regional airport in North Carolina on Thursday morning.
The Cessna C550 was registered to GB Aviation Leasing, a company owned by ex-racer Greg Biffle, according to Charlotte NBC affiliate WCNC.
The plane crashed at Statesville Regional Airport, about 40 ...Read more

Natalee Holloway killer Joran van der Sloot attempts suicide in prison
Joran van der Sloot, the Dutch citizen who has admitted to killing American tourist Natalee Holloway in 2005, appears to have attempted to end his own life in a Peruvian prison.
The 38-year-old murderer was found in critical condition with a sheet tied around his neck Saturday morning, according to local outlet La Republica. He’s serving a 28...Read more

Colorado CDL program for immigrant truckers indefinitely suspended
DENVER — Colorado’s program for issuing commercial driver licenses to immigrants with temporary legal status has been shut down for nearly two months and remains indefinitely suspended as state officials conduct an audit in response to a federal government crackdown on illegal trucking.
U.S. Transportation Secretary Sean Duffy has ordered ...Read more

Ghislaine Maxwell brings last-ditch bid to toss conviction, could impact release of 'Epstein files'
NEW YORK — Ghislaine Maxwell on Wednesday asked a federal court to throw out her sex trafficking conviction and 20-year prison sentence for aiding Jeffrey Epstein’s sexual exploitation of teenage girls.
In a habeas petition filed in Manhattan Federal Court, the former socialite — representing herself — argued new information arising...Read more

US core CPI eases to four-year low in shutdown-impacted report
Underlying U.S. inflation rose in November at the slowest annual pace since early 2021, an unexpected improvement in a report muddled by the government shutdown.
The core consumer price index, which excludes the often-volatile food and energy categories, increased 2.6% in November from a year ago, according to Bureau of Labor Statistics data ...Read more
Florida's new license plate law leads to immigration detention and a wrongful arrest in Broward County
FORT LAUDERDALE, Fla. — Justin Cuellar was driving through Davie with his father to pick up their trailer last Tuesday when a Florida Highway Patrol trooper knocked on their window.
He told them that it was difficult to see the “Sunshine” letters on their truck’s license plate and they couldn’t have anything obstructing it, Cuellar, ...Read more
Popular Stories
- Illinois mom covers 250-mile distance to reunite formerly detained immigrants with their Chicago families: 'They deserve to know somebody cares'
- Trump announces military 'warrior dividend' amid inflation woes
- Missouri legalized abortion, but most residents can't get appointments and go elsewhere
- DACA was once a lifeline for undocumented youth. It's leaving the next generation behind
- It's an open secret that some of Philadelphia's charter schools push out kids with behavioral problems, principals say