Current News
/ArcaMax

Commentary: Donald Trump wants a resurgence in European nationalism
To fix what he sees wrong in Europe, President Donald Trump has prescribed the continent’s ancient and most lethal poison — nationalism.
Nationalism is a patriotism, a love of one’s own country, that has curdled into a hatred both of other countries and of minority groups at home. In the 20 th century, nationalism was the driving force ...Read more

Ten Commandments in schools, DEI bans among 2026 'culture war' proposals in SC
COLUMBIA, S.C. — Requiring the Ten Commandments in schools, banning public diversity initiatives and restrictions on who can use which bathroom could all be topics of ideological battles waged in the South Carolina statehouse next year.
Culture war issues, including diversity, equity and inclusion policies, abortion and book bans, have shaped...Read more
She was approved for a green card after 3 decades in the US. Then ICE arrested her
LOS ANGELES — Babblejit "Bubbly" Kaur and her husband, Amarjit Singh, celebrated their 41st wedding anniversary in Long Beach in late November. The pair cradled a mint-frosted cake in their hands and beamed as their daughter, Joti, snapped pictures.
The couple endured a lot in those years, more than 30 of which have been spent in the U.S., ...Read more

Who's running the LAPD? Chief's style draws mixed reviews in first year
LOS ANGELES — When an LAPD captain stood up during a meeting this fall and asked Chief Jim McDonnell to explain the role of his most trusted deputy, Dominic Choi, other top brass in attendance waited with anticipation for the reply.
Multiple department sources, who requested anonymity to discuss the private meeting and speak candidly about ...Read more

Trump suspends US green card lottery after Brown, MIT attacks
The Trump administration halted the U.S. green card lottery program, which it said was used by the suspect in the Brown University shooting and killing of a Massachusetts Institute of Technology professor.
Homeland Security Secretary Kristi Noem said in a post on X that she’s asking U.S. Citizenship and Immigration Services to pause the ...Read more

California in for wet, white, potentially wild Christmas as Pineapple Express storm looms
A powerful Pineapple Express storm could deliver a wet, white and potentially wild Christmas to California, with the possibility of snow in the Sierra Nevada and plenty of rainfall across Southern California.
The incoming atmospheric river system is shaping up to be the strongest in years to hit the Los Angeles area on the holiday — and ...Read more

Brown University shooter found dead in New Hampshire: reports
The suspected shooter who killed two Brown University students on Saturday has been found dead in a New Hampshire storage facility, according to multiple reports.
Reports from the Associated Press and Fox News do not identify their source for the information. A press conference on the case is set to begin within minutes.
Earlier story
...Read more

NYC Council passes housing bills focused on affordability in final 2025 meeting
NEW YORK — At their final meeting of the year, New York City Council members on Thursday passed a slew of housing-related bills that would require the city to build more affordable housing for families and put local nonprofits at the front of the line for building sales.
But a spokesman for Mayor Eric Adams, who can still use his veto pen ...Read more

Mayor Adams appoints four Rent Guidelines Board members as parting punch to Mamdani
NEW YORK — Mayor Eric Adams appointed four members late Thursday to the city’s Rent Guidelines Board in a last-minute attempt to stymy Mayor-elect Zohran Mamdani’s promise of a rent freeze for stabilized tenants.
The mayor’s move comes in his last days in office. Mamdani is set to take office Jan. 1.
“We are just as committed to a ...Read more

Brown University shooter identified as former student, found dead in New Hampshire
The suspected shooter who killed two Brown University students on Saturday has been found dead in a New Hampshire storage facility.
“Tonight our Providence neighbors can finally breathe a little easier,” Providence Mayor Brett Smiley said at a 9:35 p.m. press conference. “I want to thank the people of Providence for stepping up and coming...Read more

Atlantic City Mayor Marty Small Sr. acquitted of abusing teen daughter
Atlantic City Mayor Marty Small Sr. was acquitted on Thursday of all the charges against him in connection to the alleged abuse of his teenage daughter.
The 51-year-old Democrat, who won reelection in November, had been indicted in September 2024, alongside his wife, La’Quetta Small, the city’s superintendent of schools. Both were charged ...Read more

Recently appointed Mamdani official abruptly resigns as antisemitic tweets unearthed
A top official in Mayor-elect Zohran Mamdani’s incoming administration resigned abruptly Thursday after a series of anti-Jewish tweets were uncovered, just one day after her appointment was announced.
Cat Da Costa, who would have served as Mamdani’s head of appointments in the mayor’s office, resigned hours after the social media posts ...Read more

FAA warns of military aircraft flying undetected in Caribbean
WASHINGTON — The U.S. Federal Aviation Administration has issued a notification to pilots to exercise extreme caution because of a “worsening security situation and heightened military activity” around Venezuela, as President Donald Trump ramps up pressure on Venezuelan President Nicolas Maduro.
U.S. military aircraft have been operating...Read more
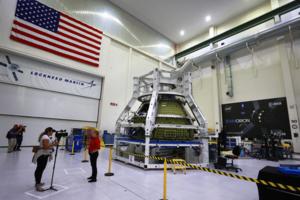
Trump reinforces NASA's moon plans, eliminates Space Council
President Donald Trump signed an executive order that aims to return astronauts to the moon through NASA’s Artemis space program with an eye toward building a permanent lunar presence.
The directive reinforces NASA’s current plans for sending Americans back to the moon by 2028 and for Americans to begin establishing the outpost by 2030. It ...Read more

TikTok says it signed agreements for a new US joint venture
TikTok’s long-delayed plan to separate from Chinese parent ByteDance Ltd. was put in motion Thursday when the video sharing sensation said it’s being bought by a group of buyers led by Oracle Corp.
TikTok Chief Executive Officer Shou Chew told employees that the company and ByteDance signed binding agreements to create a US joint venture ...Read more

CPI report with shutdown voids raises doubts about US inflation data
After long-awaited government data showed underlying U.S. inflation cooled to a four-year low in November, economists agreed on at least this much: something was off.
In a report fouled by the record-long government shutdown, inflation in several categories that had long been stubborn seemed to nearly evaporate. Chief among those were shelter ...Read more

Judge blasts ICE for defying court by holding Jamaican immigrant in 'putrid' Long Island cell
A federal judge blasted U.S. Immigration and Customs Enforcement for ignoring court orders to release a Jamaican immigrant married to a U.S. citizen whom ICE detained for days inside a “putrid and cramped” holding cell on Long Island.
Following his arrest by ICE agents on Dec. 5, Erron Clarke was subjected to “inhumane and unlawful ...Read more

Providence police seen in NH searching for Brown University shooter; authorites look into possible link to MIT professor shooting
Police in Providence, Rhode Island, and other authorities, including the U.S. Marshals, are searching on a street off Route 28 in Salem, New Hampshire, as the investigation into Saturday’s Brown University shooting developed into a multistate manhunt with possible connections to the slaying of an MIT professor in his Brookline, Massachusetts, ...Read more

New Trump administration proposals could further reduce gender-affirming care for minors in Illinois
CHICAGO — In a move that could further reduce gender-affirming care for minors in Illinois, the federal government is proposing rules that would strip Medicare and Medicaid funding from hospitals that provide such services.
The administration of President Donald Trump has been threatening since early this year to block federal funding for ...Read more

California Turning Point USA club in jeopardy after city councilwoman's controversial comments
A Northern California elected official is under scrutiny over comments she made at an after-school meeting of a conservative students club, where she attributed her daughter's sexual orientation to childhood trauma and repeated talking points criticized workplace diversity and the legacy of civil rights leader Martin Luther King Jr.
The ...Read more
Popular Stories
- Providence police seen in NH searching for Brown University shooter; authorites look into possible link to MIT professor shooting
- California in for wet, white, potentially wild Christmas as Pineapple Express storm looms
- NASCAR star Greg Biffle, his family among 7 dead in North Carolina plane crash
- Brown University shooter found dead in New Hampshire: reports
- Pope Leo XIV names Illinois Bishop Ronald Hicks as archbishop of New York