Health Advice
/Health

As bans spread, fluoride in drinking water divides communities across the US
MONROE, N.C. — Regina Barrett, a 69-year-old retiree who lives in this small North Carolina city southeast of Charlotte, has not been happy with her tap water for a while.
“Our water has been cloudy and bubbly and looks milky,” said Barrett, who blames fluoride, a mineral that communities across the nation have for decades added to the ...Read more

Organ donation: Don't let these myths confuse you
Over 100,000 people in the U.S. are waiting for an organ transplant. Unfortunately, many may never get the call saying that a suitable donor organ — and a second chance at life — has been found. It's estimated that more than 15 people die every day in the U.S. because of the lack of donor organs.
It can be hard to think about what's going ...Read more

Lawsuit alleges Obamacare plan-switching scheme targeted low-income consumers
A wide-ranging lawsuit filed Friday outlines a moneymaking scheme by which large insurance sales agency call centers enrolled people into Affordable Care Act plans or switched their coverage, all without their permission.
According to the lawsuit, filed in U.S. District Court for the Southern District of Florida, two such call centers paid tens...Read more

Arkansas led the nation in measuring obesity in kids. Did it help?
LITTLE ROCK, Ark. — Sixth-grade boys were lining up to be measured in the Mann Arts and Science Magnet Middle School library. As they took off their shoes and emptied their pockets, they joked about being the tallest.
“It’s an advantage,” said one. “You can play basketball,” said another. “A taller dude can get more girls!” a ...Read more

Commentary: The decline in American life expectancy harms more than our health
American life expectancy started dropping even before the pandemic. It’s a critical barometer of our nation’s health and a sign that all is not well in the U.S.
Much of the increase in preventable, premature death is attributable to drug overdose, which increased five-fold over the last couple decades. But this malaise is far broader, ...Read more

Tech neck is a pain in more than just the neck
The typical average adult head weighs approximately 10-12 pounds. But did you know that bending it forward at a 45-degree angle to look at a cellphone or tablet can dramatically increase your chances to have "tech neck?"
"That's like having an 8-pound bowling ball as your head. Then you have 72 pounds at your elbow and 96 pounds on your ...Read more

False offers of cash subsidies used to 'capture' health insurance customers, lawsuit alleges
A health insurance operation based in Broward County, Florida, used internet ads that falsely promised cash subsidies to sign up clients across the country and replace their agents, a lawsuit contends.
The scheme was carried out by Enhance Health LLC, TrueCoverage LLC, Speridian Technologies LLC, Number One Prospecting LLC and two individuals ...Read more
Atrium Health shared patient data with Facebook, class-action lawsuit alleges
A class-action lawsuit filed in North Carolina accuses Atrium Health of allowing Facebook and Google to access patient information online to use in targeted ads.
The plaintiffs, identified only as North Carolina-resident J.S. and Michigan-citizen J.R., allege they received spam mail and Facebook ads related to their medical conditions after ...Read more

Doctors take on dental duties to reach low-income and uninsured patients
DENVER — Pediatrician Patricia Braun and her team saw roughly 100 children at a community health clinic on a recent Monday. They gave flu shots and treatments for illnesses like ear infections. But Braun also did something most primary care doctors don’t. She peered inside mouths searching for cavities or she brushed fluoride varnish on ...Read more
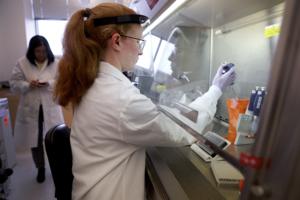
Mayo Clinic virologist offers perspective on avian influenza outbreak
Health officials around the globe, including the Centers for Disease Control and Prevention and the European Centre for Disease Control and Prevention, are monitoring the ongoing avian influenza outbreak. Also known as bird flu, the highly contagious viral disease typically spreads among birds, but can also infect livestock and, in rare cases, ...Read more

Ten doctors on FDA panel reviewing Abbott heart device had financial ties with company
When the FDA recently convened a committee of advisers to assess a cardiac device made by Abbott, the agency didn’t disclose that most of them had received payments from the company or conducted research it had funded — information readily available in a federal database.
One member of the FDA advisory committee was linked to hundreds of ...Read more

City-country mortality gap widens amid persistent holes in rural health care access
In Matthew Roach’s two years as vital statistics manager for the Arizona Department of Health Services, and 10 years previously in its epidemiology program, he has witnessed a trend in mortality rates that has rural health experts worried.
As Roach tracked the health of Arizona residents, the gap between mortality rates of people living in ...Read more

U.S. Supreme Court allows Idaho's ban on gender-affirming care to go into effect
The U.S. Supreme Court has ruled that Idaho’s ban on gender-affirming care for transgender minors can go into effect, overruling a lower court while the long-term constitutionality of the state’s law is still being litigated.
Idaho Attorney General Raúl Labrador asked the high court to allow the ban to go into effect in February, after a ...Read more

U.S. Supreme Court allows Idaho's ban on gender-affirming care to go into effect
The U.S. Supreme Court has ruled that Idaho’s ban on gender-affirming care for transgender minors may go into effect, overruling a lower court while the long-term constitutionality of the state’s law is still being litigated.
Idaho Attorney General Raul Labrador asked the high court to allow the ban to go into effect in February, after a ...Read more

Why some adults may need another dose of measles vaccine
A rising number of measles cases in the U.S. this year is raising concerns over a comeback of a disease that was declared eliminated in this country 24 years ago.
A measles report from the Centers for Disease Control and Prevention last week concluded that the spike in cases means more public health efforts are needed to increase routine ...Read more

More kids are dying of drug overdoses. Could pediatricians do more to help?
A 17-year-old boy with shaggy blond hair stepped onto the scale at Tri-River Family Health Center in Uxbridge, Massachusetts.
After he was weighed, he headed for an exam room decorated with decals of planets and cartoon characters. A nurse checked his blood pressure. A pediatrician asked about school, home life, and his friendships.
This ...Read more

Colorado has lost dozens of autism clinics as state struggles to shore up funding
For the first time in years, Jay Ortengren has seen his 16-year-old son, Ethan, reach milestone after milestone as he lives with a severe form of autism.
Ortengren and his family uprooted their lives in search of the best treatment for Ethan after he was diagnosed as a young child. Finally, they seemed to find it when they moved to Jefferson ...Read more

To close racial gap in maternal health, some states take aim at 'implicit bias'
Countless times, Kenda Sutton-El, a Virginia doula, has witnessed her Black pregnant clients being dismissed or ignored by clinicians.
One woman was told by doctors that swelling, pain and warmth in her leg was normal, despite warning the clinicians that she had a history of blood clots. Sutton-El urged her to visit the emergency room. Tests ...Read more

Ask the Pediatrician: What should I do if my child's ADHD medication is out of stock during the shortage?
If you are scrambling to get your child's attention-deficit/hyperactivity disorder prescription refilled, you are definitely not alone. Families across the U.S. have been dealing with an ADHD medication shortage first reported in October 2022 that is now well into its second year.
I've heard stories of parents and caregivers having to drive as ...Read more

Dietary choices are linked to higher rates of preeclampsia among Latinas
For pregnant Latinas, food choices could reduce the risk of preeclampsia, a dangerous type of high blood pressure, and a diet based on cultural food preferences, rather than on U.S. government benchmarks, is more likely to help ward off the illness, a new study shows.
Researchers at the USC Keck School of Medicine found that a combination of ...Read more
Popular Stories
- Why some adults may need another dose of measles vaccine
- More kids are dying of drug overdoses. Could pediatricians do more to help?
- Colorado has lost dozens of autism clinics as state struggles to shore up funding
- Atrium Health shared patient data with Facebook, class-action lawsuit alleges
- Doctors take on dental duties to reach low-income and uninsured patients