Entertainment
/ArcaMax
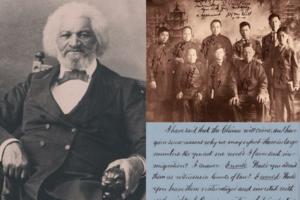
7 moments of Asian American and Black American solidarity
"Divide and conquer" is a maxim that has proven effective in myriad scenarios—negotiations and computer programming, for example. But, more insidiously, it has also been used to cement social hierarchies.
Wealthy colonial Americans used the supposed superiority of one race over another to disrupt the solidarity of those in lower income ...Read more

These states have the highest-quality home health agencies, according to patients
In an ideal world, at-home health care services would be equal no matter where a patient lives—after all, these services transfer care into the comfort of one's own home. But the reality is far from balanced.
The need for home health aides is expected to balloon over the next several years. This increased demand is in part because ...Read more

Truck-safe city parking: 4 innovations to protect cars and pedestrians
If you drive a car regularly, you've probably faced the frustration of arriving at your destination, searching for a parking spot, and coming up dry.
Big-rig truck drivers across the U.S. face that reality daily. In a survey of 11,000 drivers conducted in 2020 by the Federal Highway Administration, nearly all (98%) truckers said they have ...Read more

15 of the most inspiring actor comebacks of all time
Hollywood is known for chewing people up and spitting them out, a symptom of an industry always looking for the next big (and lucrative) thing. When an actor makes their mark or even wins an Academy Award, that's not a guarantee that their career will continue to receive consistent support.
Take, for example, Hilary Swank, one of Hollywood's...Read more

7 Asian Americans whose discoveries changed the world
Technology has rapidly advanced the speed of invention, getting cutting-edge products and treatments into peoples' hands faster. But while we consumers passively enjoy technological updates to make our lives frictionless, the many hands who touch those new innovations—the researchers, discoverers, engineers, and inventors—often go unnoticed...Read more

10 outdoor sites to learn more about Asian American, Native Hawaiian, and Pacific Islander heritage
Since the nation's earliest days, Asian Americans, Native Hawaiians, and Pacific Islanders have played vital roles in shaping the United States. They have carved out communities in isolated swamps, built the country's first transcontinental railroad, pushed back against injustices, and so much more over the past few centuries.
Though these ...Read more

5 tech advancements sports venues have added since your last event
In today's digital climate, consuming sports has never been easier. Thanks to a plethora of streaming sites, alternative broadcasts, and advancements to home entertainment systems, the average fan has myriad options to watch and learn about their favorite teams at the touch of a button—all without ever having to leave the couch.
As a ...Read more

Districts where student-teacher ratios are still behind pre-pandemic levels
In one-third of all school districts, the number of students per teacher is getting higher. Some states are grappling with ratios as high as nearly 40 students for every teacher, according to data from the National Center for Education Statistics.
Nationally, the ratio is 15.4 students for every teacher, which aligns with the decades-long ...Read more

5 charts that break down the British royal family's wealth
The British royal family is simultaneously one of the world's most well-known and secretive families. They're one of the few remaining European monarchies to have managed to continue their influence on the U.K. and beyond, even as their territories have gained independence from the British and the country's global power has diminished.
...Read more

8 emerging uses for medical cannabis
Hope is on the horizon for people who want to use marijuana to treat medical conditions.
Cannabis is currently illegal under federal law as a Schedule I drug. But in January, federal researchers recommended moving it to a Schedule III drug, which includes drugs like ketamine and testosterone that are available by prescription.
Americans ...Read more

10 pop culture moments that destigmatized weed
In the United States, the stigma surrounding cannabis, known by various names including weed, Mary Jane, or marijuana, has undergone a complex journey from being classified as a Schedule I substance with a high potential for abuse and no medical value (a decision now under review) to becoming commonplace in modern culture.
Throughout much of...Read more

10 of the best places in the US to see the northern lights in 2024
Astronomers predict this year will be the best in the last decade to see the northern lights. We have the sun's current solar cycle to thank for the stronger aurora borealis in 2024. Scientists say the sun is hitting its "solar maximum," or the highest activity rate during its current solar cycle, meaning more frequent and brighter northern ...Read more

Only half of Gen Z say they are thriving, less than millennials at the same age
Young Americans are less optimistic these days, but none more so than Generation Z.
Less than half (47%) of Gen Zers said they were thriving, according to a survey conducted by Gallup and the Walton Family Foundation. The survey asked Americans to rate their current and future lives out of 10, with people classifying as "thriving" if they ...Read more

How much do prices for health services vary within a city?
Health care prices are notoriously opaque in America. A 2022 InstaMed survey reported that 71% of consumers found their medical bills confusing, while 76% received an unexpected charge.
Congress introduced a number of reforms in recent years designed to help people figure out how much various medical services actually cost. As of Jan. 1, ...Read more

When teachers quit for other jobs, how is life outside of the classroom?
Reports of teachers leaving their jobs in search of more stability and higher pay are not uncommon, but is the grass greener on the other side?
HeyTutor analyzed data from the National Center for Education Statistics, published in December 2023, to show how teachers feel about leaving careers in education. Data includes results from the ...Read more

10 celebrities who have broken into the cannabis business
Gone are the days of the simple choice of smoking a joint or munching on a pot brownie to consume weed. The cannabis industry has made inroads just about everywhere you can imagine—think products like coffee pods, bath bombs, and toothpaste. As recreational and medicinal cannabis use becomes legal in more states across the U.S., companies are...Read more

These countries are among the biggest gold consumers
Gold has been a desirable commodity for thousands of years, dating back to ancient civilization.
In Rome, Julius Caesar gifted 200 gold coins to each of his soldiers to celebrate their victory against Gaul. Gold production and consumption have grown continually through modern times. In fact, most gold worldwide—more than 90%—has been ...Read more

1 in 4 Americans are physically inactive. Here's how that impacts you as you age.
In 2024, nearly half (48%) of American adults made a New Year's resolution to improve their fitness, according to a Forbes Health/OnePoll survey.
It's a good goal—because Americans aren't doing it nearly enough.
Nearly 1 in 4 American adults are not getting the suggested two days of muscle training and 150 minutes of moderate exercise ...Read more

Charging toward net zero: The environmental factors electric vehicles don't fix
The U.S. has ambitious goals to curb climate change in the coming decades—and electric vehicles feature heavily in that plan.
EV vehicles represent an immense leap in automotive industry capabilities made possible by computer chips and battery technology advancements, further nudged by government incentives. But research and current ...Read more

Decades of design: How American interior design trends reflect our history
From decade to decade, our personal spaces have reflected the times, impacted by the events of each era that influence not only the nation's temperament, but also the availability of materials and objects to furnish homes.
To relive the most memorable design movements over the last 100 years, Living Spaces traveled back in time via archival ...Read more