Current News
/ArcaMax

Vulnerable Florida patients scramble after abrupt Medicaid termination
TAMPA, Fla. – Esther JeanBart leaned over her son’s wheelchair, caressing his face and trying to make him giggle. Gianni JeanBart was under the weather, but still his eyes rolled toward her and his mouth widened, cracking a smile.
Esther JeanBart said she has missed the sound of Gianni’s voice the most. In 2017, the U.S. Marine was in a ...Read more

Supreme Court tackles homelessness crisis. What that means for California
WASHINGTON — The Supreme Court is poised to hear its most important case ever on the homelessness crisis, and to decide whether cities in California and the West may enforce laws against camping on sidewalks or other public property.
Homelessness has often been cited as the most intractable problem for cities in the West, and it has grown ...Read more

Israel launches missile strikes on Iran, US officials say
Israel launched a retaliatory strike on Iran less than a week after Tehran’s rocket and drone barrage, according to two U.S. officials, but Iranian media appeared to downplay the incident in the hours that followed the initial reports.
An explosion was heard early Friday in Iran’s central city of Isfahan, the country’s semi-official Fars ...Read more

Israel launches missile strikes on Iran, US officials say
Israel launched a retaliatory strike on Iran less than a week after Tehran’s rocket and drone barrage, according to two U.S. officials, raising fears of a widening conflict across the Middle East.
An explosion was heard early Friday in Iran’s central city of Isfahan, the country’s semi-official Fars news agency reported. Nuclear ...Read more

Israel launches missile strikes on Iran, US officials say
Israel launched a missile strike on Iran less than a week after Tehran’s rocket and drone barrage, according to two U.S. officials.
An explosion was heard Friday in Iran’s central city of Isfahan, the country’s semi-official Fars news agency reported, as concerns mounted about Israeli retaliation.
Flights were suspended in Isfahan and ...Read more

Pennsylvania House Democrats take step toward expelling state Rep. Kevin Boyle
HARRISBURG, Pa. — A top House Democratic leader took a first step Thursday toward expelling State Rep. Kevin Boyle from the state House, as the lawmaker faces criminal charges and his family says he’s suffering from a serious mental health condition.
Democratic House Majority Leader Matt Bradford, in response to Boyle’s situation, ...Read more
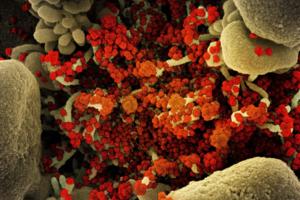
It's taken 100 scientists two years to rename airborne viruses after COVID-19 mistakes
Airborne viruses will be called “pathogens that transmit through the air” under new terminology the World Health Organization hopes will end a scientific rift that hampered the early response to COVID-19.
After two years of consultations involving over 100 scientists, a WHO-led working group agreed to the term to describe diseases caused ...Read more

Blasts heard near air base in Iran's Isfahan, news agency reports
An explosion was heard early Friday in Iran’s central city of Isfahan, the semi-official Fars news agency reported, citing local sources.
The cause of the blast is unknown, according to the report. An Iranian army air base and Isfahan’s airport are reportedly close to the explosion site, Fars said. Global oil and gold prices rose.
...Read more

Full jury selected for Trump hush money trial
NEW YORK — The 12 New Yorkers who will decide whether or not Donald Trump is a felon before this year’s presidential election were seated during a dramatic day of proceedings Thursday, leaving the court to find five alternates before his historic hush money trial begins in earnest.
“We have our jury,” Manhattan Supreme Court Justice ...Read more

Gov. Jared Polis signs bill sending $24 million to Colorado schools seeing influx of immigrant students
DENVER — Colorado will distribute $24 million in one-time funding to public school districts and charter schools impacted by the unprecedented influx of immigrant students who arrived after the annual October headcount that determines districts’ state funding.
Gov. Jared Polis on Thursday signed the bipartisan bill, HB24-1389, authorizing ...Read more

Karen Read murder case still 4 jurors short of ready for trial
BOSTON — Attorneys on Thursday selected two more in the third batch of potential jurors in the white-hot Karen Read murder case at Norfolk Superior Court, but didn’t get enough for trial and will have to interview at least one more batch.
Jury selection began Tuesday in Norfolk Superior Court in Dedham with more than 90 candidates. ...Read more

Democratic National Convention organizers leaning on locals to handle possible migrant surge in August
CHICAGO — Anticipating Chicago will see a surge of buses bearing migrants from the southern border ahead of the Democratic National Convention in August, organizers say they’re relying on Mayor Brandon Johnson and Illinois Gov. J.B. Pritzker to come up with a plan to stave off any ensuing potential chaos.
So far, Johnson and Pritzker have ...Read more

ks-NEV-REPRODUCTIVE-FREEDOM // Nevada Supreme Court rules reproductive freedom petition can move forward
A petition to protect reproductive freedoms in the Nevada Constitution can advance to the November ballot, the State Supreme Court ruled Thursday.
Justices determined the District Court made errors in an earlier ruling saying, “the initiative petition has a single subject: the establishment of a fundamental right to reproductive freedom. All ...Read more

NYPD arrests students, clears Columbia University campus of pro-Palestinian protest encampment
NEW YORK — NYPD officers arrested more than 100 Columbia University students Thursday after groups protesting the war in Gaza refused to take down a two-day encampment zone.
Hundreds of cops flooded the campus at the request of the university president, with buses on standby to transport demonstrators downtown for trespassing. Other students,...Read more

Embryos were accidentally destroyed at Newport Beach fertility clinic, lawsuits claim
An Orange County, California, fertility clinic accidentally destroyed embryos after they came in contact with hydrogen peroxide while an employee was cleaning an incubator, according to a pair of lawsuits filed by two couples on Thursday.
The couples, who failed to become pregnant after the embryos were implanted in late January, accuse FPG ...Read more

DA files involuntary manslaughter charges against three Alameda, California, officers in death of Mario Gonzalez
OAKLAND, Calif. — Alameda County District Attorney Pamela Price on Thursday announced criminal charges against three police officers involved in the 2021 death of Mario Gonzalez, who stopped breathing while being pinned to the ground by multiple officers.
Price is charging three Alameda Police Department officers — Eric McKinley, James ...Read more

Nevada Supreme Court rules reproductive freedom petition can move forward
A petition to protect reproductive freedoms in the Nevada Constitution can advance to the November ballot, the State Supreme Court ruled Thursday.
Justices determined the District Court made errors in an earlier ruling saying, “the initiative petition has a single subject: the establishment of a fundamental right to reproductive freedom. All ...Read more
News briefs
Kennedy family endorses Biden in bid to counter RFK Jr.
WASHINGTON — President Joe Biden called it an “incredible honor” as he received endorsements from more than a dozen members of the Kennedy family, in a public show of force aimed at undercutting the presidential campaign of independent Robert F. Kennedy Jr.
Biden, flanked by his ...Read more

Rep. Ilhan Omar's daughter among students suspended at Columbia over pro-Palestinian encampment
NEW YORK — The daughter of Rep. Ilhan Omar of Minnesota, a vocal Democrat sharply critical of Israel, was among at least three students suspended Thursday over a pro-Palestinian encampment at Columbia University.
Omar, who made history as one of the first two Muslim women elected to Congress and has been a sharp critic of the war in Gaza, ...Read more

'You can't say that to a woman in 2024': Texas judge's words called racist, misogynistic
FORT WORTH, Texas — Residents and members of local civil rights organizations gathered Thursday to denounce Tarrant County Judge Tim O’Hare’s recent treatment of Commissioner Alisa Simmons, which they described as racist, misogynistic, and publicly intimidating.
The news conference sprang from an exchange between O’Hare and Simmons at a...Read more
Popular Stories
- Full jury selected for Trump hush money trial
- Democratic lawmaker takes the bait on Marjorie Taylor Greene 'troll' amendment
- 'You can't say that to a woman in 2024': Texas judge's words called racist, misogynistic
- Recognizing racist past, Tampa will create reconciliation committee
- NYC squatters got engaged, spent big after stuffing slay victim in duffel bag, prosecutors say