Current News
/ArcaMax

LA ethics panel approves fine for former CBS exec Leslie Moonves over interference with LAPD investigation
LOS ANGELES — Former CBS President Leslie Moonves will pay $15,000 to settle a Los Angeles city ethics complaint over his role in an alleged cover-up of sexual assault accusations against him.
The city’s Ethics Commission unanimously approved the settlement Wednesday after previously rejecting a proposal for $11,250 in fines as too low.
...Read more

Salmonella outbreak causes Trader Joe's to recall a Miami firm's herbs in 29 states
Trader Joe’s took herbs made by a Miami area company off the shelves of stores in 29 states and issued a recall of those already sold after a CDC and FDA investigation links the herbs to a salmonella outbreak.
Here’s what you need to know.
What basil did Trader Joe’s recall?
This recall involves Infinite Herbs Organic Basil from Feb. 1 ...Read more

Clark County GOP chair arrested, faces domestic battery charge
Clark County Republican Party Chairman Jesse Law was arrested last weekend and faces a domestic battery charge, according to Metro booking records.
Law was arrested Sunday and faces a charge of domestic battery first offense, according to Las Vegas Justice Court records.
Law declined to comment Wednesday evening and referred requests to his ...Read more

San Diego Unified OKs its first affordable housing development on school property
SAN DIEGO — San Diego Unified School District officials took a key step forward this week with their plan to help ease the local housing crisis by letting developers build large rent-restricted apartment complexes on excess school property.
District trustees selected a developer to transform the former campus of Central Elementary in City ...Read more

House bill gives up to a year to sell TikTok; eyes Russian assets
WASHINGTON — Speaker Mike Johnson late on Wednesday unveiled a modified version of the previously House-passed legislation targeting TikTok that would give Chinese owner ByteDance up to a year to divest the app, an increase from the six months given in the earlier version.
The bill, the fourth part of a package of measures released Wednesday ...Read more

Pa. state Rep. Kevin Boyle evades arrest; US Rep. Brendan Boyle says his brother has 'serious mental health condition'
PHILADELPHIA — State Rep. Kevin Boyle had not yet turned himself in to Philadelphia police as of Wednesday evening, a day after a warrant was issued for his arrest on charges related to violating a protection from abuse order.
As Boyle eluded arrest, his older brother, U.S. Rep. Brendan Boyle, said the reemergence of a mental health condition...Read more

Attorneys for Bryan Kohberger file alibi defense in Idaho student homicide case
BOISE, Idaho — Attorneys for Bryan Kohberger met the Wednesday deadline to file their client’s alibi defense in the murder case against him in the deaths of four University of Idaho students in November 2022.
In a 10-page filing near the end of the day, Kohberger’s attorneys added extra details about their client’s whereabouts the early...Read more

Antisemitic hate crimes in NYC spiked in first months of 2024
NEW YORK — Antisemitic hate crimes in New York City have spiked as conflict continues to rage in the Middle East.
As of Sunday, there have been 96 hate-fueled incidents targeting Jewish people, according to NYPD stats. The figure marked a 45% uptick compared with the same time frame last year, when cops investigated 66 antisemitic hate crimes...Read more
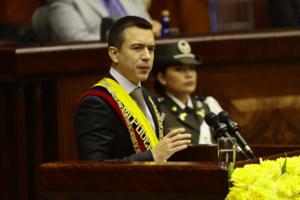
Ecuador President Daniel Noboa shuts down nation on electricity crisis
Ecuador’s President Daniel Noboa ordered businesses and government offices to shut down Thursday and Friday amid a crippling lack of electrical power ahead of a key national referendum scheduled for Sunday.
Noboa blamed the unprecedented measure on drought, but also sabotage, without offering evidence. The energy crisis comes on the heels of ...Read more
High profile for-profit Bay Area coding school BloomTech hit by feds for allegedly tricking students
High-profile Bay Area coding school BloomTech, which touts “dream” technology jobs at companies such as Google and Amazon, has been sanctioned by federal authorities for allegedly deceiving students about loan costs and making false claims about graduates’ hiring rates.
The Consumer Financial Protection Bureau in an order banned the ...Read more

NYC mayoral aide Timothy Pearson sued by second retired sergeant over sex harassment controversy
NEW YORK — Top New York City mayoral aide Timothy Pearson is facing a new lawsuit linked to his alleged sexual harassment of retired Sgt. Roxanne Ludemann that includes allegations of a curious remark about the aborted construction of a migrant shelter.
Retired Sgt. Michael Ferrari alleges in a lawsuit filed Wednesday in Manhattan Supreme ...Read more

Stepson of former 'Real Housewives of New Jersey' star Siggy Flicker arrested in NYC for role in Jan. 6
The stepson of former “Real Housewives of New Jersey” star Siggy Flicker was arrested in connection to his alleged role in the Capitol riots on Jan. 6, after Flicker reportedly shared evidence of him attending on social media.
Tyler Campanella was detained Wednesday in New York City, and is now facing five misdemeanor charges related to ...Read more

Mayor Brandon Johnson slams uphill effort to recall Chicago mayors
CHICAGO — Mayor Brandon Johnson on Wednesday blasted a nascent effort to establish a legal tool for voters to recall Chicago mayors, calling it “disingenuous” and saying it is backed by “extreme right wing” political rivals.
The mayor’s comments came after a Lakeview resident earlier this month created a political committee with the...Read more
News briefs
Bob Menendez poised to blame his wife in bribe case defense
WASHINGTON — U.S. Senator Bob Menendez is prepared to blame his wife at his bribery trial for withholding information from him about gifts they allegedly accepted from businessmen seeking favors, a newly unsealed court document shows.
The revelation came Tuesday in a portion of a ...Read more

SpaceX tallies 1st of 2 launches over 2 days from Space Coast
ORLANDO, Fla. — SpaceX launched Wednesday evening the first of a pair of Space Coast rockets in two days, both carrying batches of the company’s Starlink satellites.
A Falcon 9 rocket carrying 23 of the internet satellites for SpaceX’s growing constellation lifted off at 5:26 p.m. Eastern time from Kennedy Space Center’s Launch Pad 39-A...Read more

Dozens of recreational boats use alternate channel to pass collapsed Key Bridge for first time
BALTIMORE — Chuck and JoAnn Anderika were up before dawn Tuesday to bring their sailboat back home.
The Anderikas set out around 6 a.m. from Solomons Island, headed for Baltimore. The couple wanted to ensure they made it in time to take advantage of a one-hour window for recreational boats to pass by the wreckage of the Francis Scott Key ...Read more

Cannabis enforcement deal is locked down in NY State budget
NEW YOKR — A legislative package boosting New York City in its battle against the estimated 2,500 unlicensed cannabis shops operating citywide has been secured in state budget negotiations, lawmakers said Wednesday.
The plan to fight illegal cannabis stores, one of the most closely watched policy elements in the state budget, would deploy a ...Read more

Salem's Satanic Temple pipe bomb arrest: Man accused of throwing explosive onto porch
BOSTON — FBI agents have nabbed an Oklahoma man accused of throwing a pipe bomb onto the porch of the Satanic Temple in Salem.
Sean Patrick Palmer, 49, has been charged with using an explosive to cause damage to a building used in interstate or foreign commerce.
Palmer was arrested on Wednesday, and will make an initial appearance in the ...Read more

Livery driver advocate offers $5,000 reward after wave of Uber, Lyft robberies
NEW YORK — A New York City livery and taxi driver advocate is offering a $5,000 reward to anyone with information that can help cops make arrests in a string of recent attacks and carjackings among working drivers.
“We are outraged that, in seven days, we have had upwards of six armed robberies,” Fernando Mateo, founder of the New York ...Read more

Alaska Senate to set aside extra school funding after warning from the feds
JUNEAU, Alaska — The Alaska Senate is planning to set aside around $15 million in its draft budget in extra school funding. That's because the federal government says state funding was not adequate for the highest-need schools during the COVID-19 pandemic.
The 2021 American Rescue Plan Act gave over $125 billion to schools across the nation ...Read more
Popular Stories
- Journalist who accused NPR of liberal bias resigns from the network
- Homelessness in San Diego County has now risen every month for 2 straight years
- Trump complains jury selection moving too fast in Manhattan hush money trial
- Foreign aid supplemental readied in House amid backlash
- DC judge orders Missouri man to jail for violating probation in Jan. 6 case