Current News
/ArcaMax

Recognizing racist past, Tampa will create reconciliation committee
TAMPA, Fla. — More than three years after the Tampa City Council formally apologized for the city’s racist past, the body unanimously approved the formation of a committee tasked with examining and addressing persistent inequities in Florida’s third-largest city.
The 13-member Race Reconciliation Committee will make policy recommendations...Read more

Democratic lawmaker takes the bait on Marjorie Taylor Greene 'troll' amendment
WASHINGTON — When Georgia Republican Rep. Marjorie Taylor Greene used a typically under-the-radar legislative process to send political messages Wednesday about foreign aid funding bills, one of her Democratic colleagues decided to strike back.
Greene filed a flurry of amendments to the Ukraine aid bill with the House Rules Committee, ...Read more

Reintroduced wolves kill 4 yearling cattle in latest of string of livestock attacks in Colorado
DENVER — Wolves killed several yearling cattle in north-central Colorado this week, bringing the total number of wolf kills of livestock this month to six.
Colorado Parks and Wildlife on Thursday confirmed that wolves killed three yearlings on a Grand County ranch between Monday night and Tuesday morning. The carcasses were discovered ...Read more

Rep. Ilhan Omar's daughter among students suspended at Columbia over pro-Palestinian encampment
NEW YORK — The daughter of Rep. Ilhan Omar of Minnesota, a vocal Democrat sharply critical of Israel, was among at least three students suspended Thursday over a pro-Palestinian, two-day encampment at Columbia University.
Omar grilled Columbia administrators Wednesday on protections for students protesting the war in Gaza.
Isra Hirsi, a ...Read more

Calexico resoundingly ousts town's first transgender mayor and a council ally
LOS ANGELES — Voters in Calexico have resoundingly ousted the first out transgender member of the City Council and her council ally after a bitter recall campaign rife with accusations of transphobia and political cronyism in the struggling city on the U.S.-Mexico border.
Nearly 74% of voters in the April 16 special election supported the ...Read more

Indoctrination and gender ideology: A look at Moms for Liberty's claims about NC schools
RALEIGH, N.C. — National and local leaders of Moms for Liberty came to Raleigh this week to promote a message that parents have to fight against indoctrination of their children by public schools.
Panelists at the Town Hall voiced concerns on issues such as a rise in school crime and teacher turnover and the difficulties of parents getting ...Read more

US blocks full UN membership for Palestinians
WASHINGTON — The United States is once again opposing Palestinian efforts to gain full membership in the United Nations.
The U.S. vetoed a Palestinian membership application Thursday, ending the latest debate on the issue at the U.N. Security Council and again squashing Palestinian statehood aspirations, at least for now.
Despite U.S. ...Read more

Biden administration resumes deportation flights to Haiti amid ongoing violence
MIAMI — Dozens of Haitians expelled from the United States arrived back in Haiti on Thursday in the Department of Homeland Security’s first deportation flight since an ongoing gang insurgency forced the Biden administration to halt a flight with deportees and order the evacuation of Americans.
Haiti’s Office of National Migration said it ...Read more
Most Alaska students are behind in math, science and language arts, latest statewide assessments show
ANCHORAGE, Alaska — The majority of Alaska students scored below grade level proficiency in statewide math, science and language arts assessments taken last spring — even after the state lowered the standard for what is considered proficient.
The latest results of the Alaska System of Academic Readiness, known as AK STAR, were released ...Read more

Iran tells UN it's ready to de-escalate if Israel stops 'adventurism'
Iran is prepared to de-escalate tensions with Israel provided that it agrees to stop further military moves against Tehran’s interests, Foreign Minister Hossein Amir-Abdollahian said at the United Nations.
“Iran’s legitimate defense and countermeasures have been concluded,” Amir-Abdollahian told the U.N. Security Council Thursday. ...Read more

Russia to hire contract soldiers in bid to avoid unpopular draft
Russia is preparing to enlist more contract soldiers as it presses its invasion of Ukraine, aiming to avoid at least for now another mass call-up that could undermine popular support for the war.
The Kremlin is anxious not to repeat the September 2022 mobilization, which shook public confidence and triggered an exodus of as many as a million ...Read more

Buttigieg to visit Miami to rally support for Biden's reelection campaign
MIAMI — U.S. Secretary of Transportation Pete Buttigieg will headline a campaign stop in Miami for President Joe Biden’s reelection bid on Friday.
Buttigieg, a former mayor of South Bend, Indiana, and one-time presidential contender, is expected to join several local mayors in Miami-Dade County, including Miami Gardens Mayor Rodney Harris, ...Read more

Prince Harry could lose key royal post after renouncing UK residency
To the likely disappointment of Prince Harry haters, he may not lose his Duke of Sussex title following news Wednesday that he has renounced his British residency. But there are questions about whether he could — or should — lose an important royal post since he now calls the United States his new home country.
According to British law, ...Read more

NYC squatters got engaged, spent big after stuffing slay victim in duffel bag, prosecutors say
NEW YORK — The young squatter couple accused of beating a Manhattan woman to death and stuffing her body in a duffel bag went on a wild shopping spree, got engaged while on the lam and even bought a diamond ring with the victim’s credit card to seal the deal, authorities said Thursday.
After fleeing to Pennsylvania and crashing the victim�...Read more

Leavenworth prosecutor, state lawmaker weighing runs for Congress as Kansas rep LaTurner exits
U.S. Rep. Jake LaTurner’s sudden announcement Thursday that he won’t seek reelection upended the race for Kansas’ 2nd Congressional District, with Leavenworth County Attorney Todd Thompson and Kansas House Majority Leader Chris Croft both weighing a candidacy.
“I appreciate what Jake’s done. I really am going to have to look into it. ...Read more

Karen Read trial: 3rd day of jury selection sees a pool of 57 potential jurors
BOSTON — Attorneys on Thursday have begun interviewing a third batch of potential jurors in the white-hot Karen Read murder case at Norfolk Superior Court.
The pool for today was significantly smaller than the prior two days of the jury selection, which began on Tuesday. While the other days had 90 or more potential jurors each, Thursday saw ...Read more

Dunleavy lays out efforts to preserve ability to spend public funds at private and religious schools
ANCHORAGE, Alaska — In the wake of a court decision that struck down key statutes governing Alaska's public homeschooling programs, Gov. Mike Dunleavy said Wednesday that he would not immediately seek to advance new statutes or regulations ensuring the programs can continue.
Anchorage Superior Court Judge Adolf Zeman ruled last week that the ...Read more

DeSantis signs school chaplains bill opposed by pastors, Satanists, ACLU
KISSIMMEE, Fla. — Gov. Ron DeSantis signed a bill into law Thursday allowing volunteer chaplains to counsel students in public and charter schools, despite warnings from a pastors group, the ACLU and the Satanic Temple that it would violate the First Amendment.
“There are some students (who) need some soul prep,” said DeSantis, who signed...Read more

Legislation would ban most uses of toxic forever chemicals within a decade
Despite widespread understanding of the health and environmental damages caused by forever chemicals, manufacturers continue to win federal approval to synthesize new versions of the toxic compounds with little, if any, government oversight.
U.S. Sen. Dick Durbin wants to begin shutting off the tap by outlawing per- and polyfluoroalkyl ...Read more
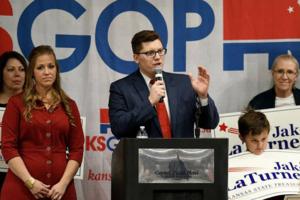
Kansas Congressman Jake LaTurner won't seek reelection, creating race for open seat
U.S. Rep. Jake LaTurner, a Republican who represents Kansas’ 2nd District, announced Thursday he won’t seek reelection, creating another open race in a furious partisan fight for control of the House.
LaTurner, 36, was first elected to the House in 2020. In a statement, LaTurner said it was time to “pursue other opportunities and have the...Read more
Popular Stories
- 5 years after the the Mueller Report into Russian meddling in the 2016 US election on behalf of Trump: 4 essential reads
- 'Shame on them': How police fumbled the case of gymnastics coach accused of sex abuse
- Juror too frightened to serve excused from Trump hush money trial
- Billions of cicadas are about to emerge from underground in a rare double-brood convergence
- Democrats prepare to ride to Johnson's rescue, gingerly